Comprehensive and Detailed Explanation From Exact Extract–Based NCC C-EFM References:
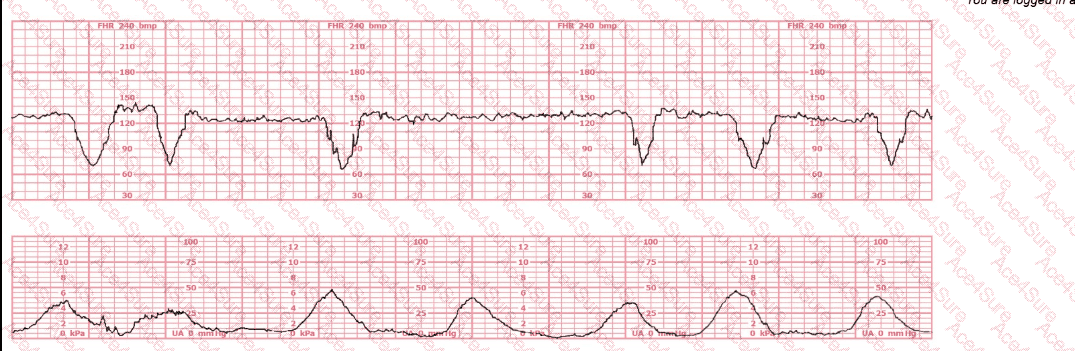
The tracing clearly shows recurrent deep variable decelerations, characterized by:
Abrupt onset (<30 sec)
Sharp V-shape
Rapid descent and ascent
Depth exceeding 60–70 bpm drops
Occurring with most contractions
This pattern is highly consistent with cord compression, which is the physiologic basis of variable decelerations. According to NCC, NICHD, AWHONN, Miller, and Menihan, recurrent (≥50% of contractions) deep variables with slow return to baseline indicate fetal compromise and require targeted intervention.
The patient has already been repositioned, so first-line management has failed. NCC emphasizes that the next recommended intervention for recurrent variable decelerations, particularly when maternal repositioning is ineffective, is amnioinfusion. This intervention relieves cord compression by restoring fluid around the umbilical cord.
Why the other choices are incorrect:
A. Apply a spiral electrode – NOT appropriate
Spiral electrodes improve signal quality but do not treat cord compression.
The tracing is already clearly interpretable, and the issue is physiologic, not technical.
B. Decrease the oxytocin – Not the best next step
Decreasing oxytocin is appropriate when tachysystole is contributing to fetal intolerance.
This strip shows normal contraction frequency (about every 2–3 minutes) and no tachysystole.
Thus, reducing oxytocin alone will not relieve cord compression.
C. Perform an amnioinfusion – CORRECT
NCC-approved references repeatedly state:
For recurrent variable decelerations that persist after maternal repositioning, amnioinfusion is recommended to reduce the frequency and depth of decelerations.
It can improve fetal oxygenation, decrease cord compression, and reduce the need for operative delivery.
It is the intervention most directly targeted to the pathophysiology of this pattern.
Therefore, C. Perform an amnioinfusion is the correct next management step.
[References:NCC C-EFM Candidate Guide (2025); NCC Content Outline; NICHD FHR Interpretation System; AWHONN Fetal Heart Monitoring Principles & Practices; Miller’s Fetal Monitoring Pocket Guide; Menihan Electronic Fetal Monitoring; Simpson & Creehan Perinatal Nursing; Creasy & Resnik Maternal–Fetal Medicine., , , ]